Objectives:
- Define AAMI ST 79:2017
- Explain how AAMI ST 79:2017 impacts quality assurance standards for assessing cleaning processes
- Apply sterile processing procedures for increased quality and control for assurance standard
Since hospitals first started monitoring and testing the sterilization process for surgical instruments more than 50 years ago, a lot has changed.
For one thing, technological advances in biological indicators made it possible to get results in less than 30 minutes, meaning hospitals could easily monitor steam and hydrogen peroxide sterilization more frequently. In fact, most hospitals are now performing every load monitoring (ELM) instead of daily monitoring for sterilization, going above and beyond what the standards recommend because of these product advances.
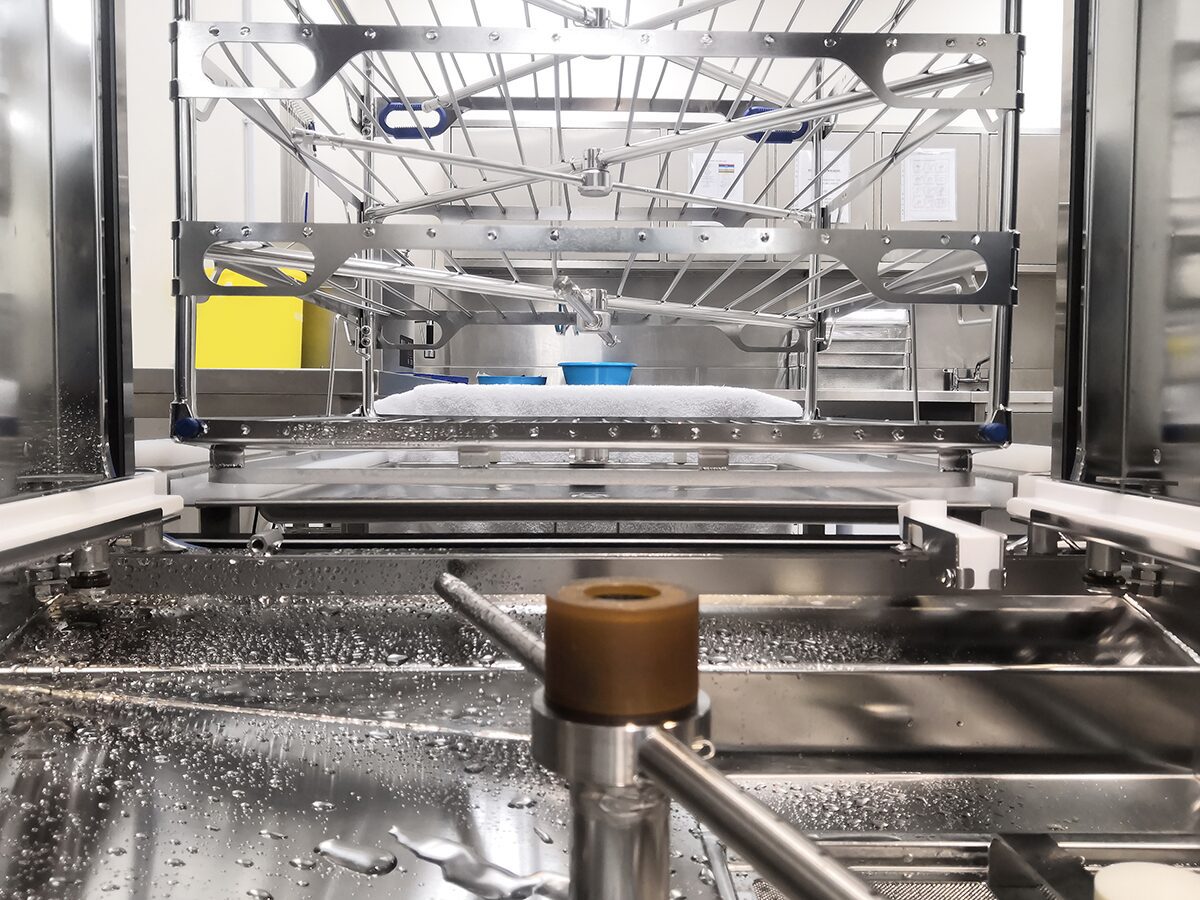
Our industry also has many products available today for monitoring cleaning processes. There are tests available to monitor mechanical cleaning equipment efficacy as well as to detect residuals on instruments. Borescopes are available to inspect the internal channels of medical devices. Gone are the days when visual inspection with the unaided eye on exterior surfaces is the only means of assessing if a device is clean.
If most hospitals are exceeding the recommendations for monitoring sterilization, what do the standards recommend for evaluating cleaning processes to ensure instruments are clean prior to sterilization?
AAMI ST 79:2017 states that verification testing should be performed on all mechanical cleaning equipment as a part of an overall quality assurance program. Mechanical cleaning equipment should be tested upon installation, each day it is used, when evaluating and changing cleaning solutions and after major repairs. (AAMI, 2017)
It is vital that the verification tests used pose a consistent, repeatable challenge to the equipment and provide real time feedback. Using a standardized test soil is a reliable way to test the functionality of the mechanical cleaning equipment. These tests should be easy to use, read, and be validated to ensure the critical parameters of the process are being measured. (AAMI, 2017) The critical parameters for a washer-disinfector include temperature, time, and presence of chemistry and the parameters for an ultrasonic include cavitation, time, temperature, and presence of chemistry. In other words, the test device used to challenge the mechanical equipment should be measuring the ability to test the critical parameters of the equipment. In some cases, it may be necessary to use two different tests for the ultrasonic, so all critical parameters are measured.
It is important to reference the instruction for use for washer tests for correct positioning and placement in the washer and ultrasonic. Several washer tests recommend that each level of a multi-level rack be tested. This makes sense because it is possible for a test placed on the top shelf of a multi-level rack to pass while the test placed on the middle shelf fails. The functionality of the spray arms is critical. If a spray arm is clogged or not spinning the instruments will not be adequately exposed to the cleaning chemistries and rinse water. Only testing the first load of the day, using 1 rack of an inventory of many, could mean future loads are compromised. Documenting the placement of the tests and identifying the rack aids in investigating the reason for a washer test failure.
Like sterilizers, washers can be programmed with different cycles. AAMI recommends that all programmed cycles in use be tested. For example, if a hospital has an eye instrument cycle and a standard cycle programmed, each of these cycles should be tested. Different chemicals, dosing, water temperature, and washing times can impact how well a cycle cleans.
The one area that is often overlooked but is recommended as part of a good quality control program is the reviewing of the washer-disinfector cycle printouts. AAMI ST79:2017 states that the printouts from the washer-disinfector, if available, should be reviewed and initialed after each load to ensure the washer completed all required phases of the cycle. In a busy department it is easy to overlook the cycle completion message on the screen, reviewing and retaining the printout provides evidence that parameters were met. To facilitate printout retention, washer disinfectors can interface to your tracking software, so the printout is automatically downloaded. Scanning instrument sets to a specific washer, documenting the results of the cycle, and capturing the printout is comprehensive documentation that allows for full traceability. It only makes sense that if the standards recommend reviewing the printout, then the instruments in each cycle should be documented.
A comprehensive quality assurance program can also include directly testing individual instruments for residual soils. These tests should be rapid, easy to use, accurate, repeatable, and sensitive to realistic benchmarks such as protein, carbohydrate, hemoglobin, adenosine triphosphate (ATP) levels. (AAMI, 2017) At some interval, individual instruments, especially complex instruments with crevices and lumens, should be checked for residual soil. In 2014, Michelle Alfa and Nancy Olson published a study comparing the ability of three different commercially available cleaning indicators to detect suboptimal washing conditions. During this study, Alfa identified that even with suboptimal washing conditions such as a lack of detergent, the instruments looked clean with visual inspection. Visual inspection of instruments without the aid of magnification or a borescope cannot be relied upon to identify inadequate cleaning. Commercially available cleaning indicators are designed to pick up inadequate cleaning results because they measure the most critical deficiencies.
For cleaning equipment to function properly, it must be maintained properly. It is important to make sure that all mechanical cleaning equipment is inspected and maintained per the manufacturer’s instructions. For washer-disinfectors, sterile processing personnel should be verifying that the spray arms are turning freely and are not clogged, strainer screens are clean, and external surfaces are not soiled. The daily and weekly maintenance tasks along with the regular preventive maintenance should be documented and all records retained.
In order to assess personnel performance, a department should have defined cleaning policies and procedures based on medical device manufacturers’ instructions and published recommendations. Instructions for use should be available for the staff to reference when working in the decontamination area. Many tracking software’s available on the market, allow for IFUs to be added for direct reference. Auditing staff performance by observing how they are cleaning medical devices and loading the equipment are a means to monitor personnel competencies which impact quality.
As you can see, a good quality control program in the sterile processing department, specifically for cleaning processes, should include objective verification methodologies that assess and verify the performance of the mechanical cleaning equipment and check for any residual contaminants on medical devices following the cleaning process. With all the variables and risks inherent in the cleaning process it will be interesting to see if ELM becomes the norm for monitoring each washer cycle much like the shift we saw with sterilization. We have come a long way with quality control in the sterile processing world. Therefore, it’s important to look at the quality assurance program in your institution and make sure it is comprehensive.
Take the Quiz to Receive Your CE Credits!
RESOURCES:
ANSI/AAMI ST79:2017. Association for the Advancement of Medical Instrumentation (AAMI)
Performance Management & Quality Improvement. CDC. https://www.cdc.gov/publichealthgateway/performance/index.html
Performance Management: Turning Point. Public Health Foundation. http://www.phf.org/programs/turningpoint/Pages/Turning_Point_Performance_Management_Refresh.aspx
Process. A Publication of the International Association of Healthcare Central Service Material Management. May/June 2020. www.iahcsmm,org
Quality Audit – A Tool for Continuous Improvement and Compliance. https://www.mastercontrol.com/gxp-lifeline/quality_audit_tool_compliance_0810/